5th Circuit’s Poliner Decision Boosts HCQIA Immunity
August 1, 2008
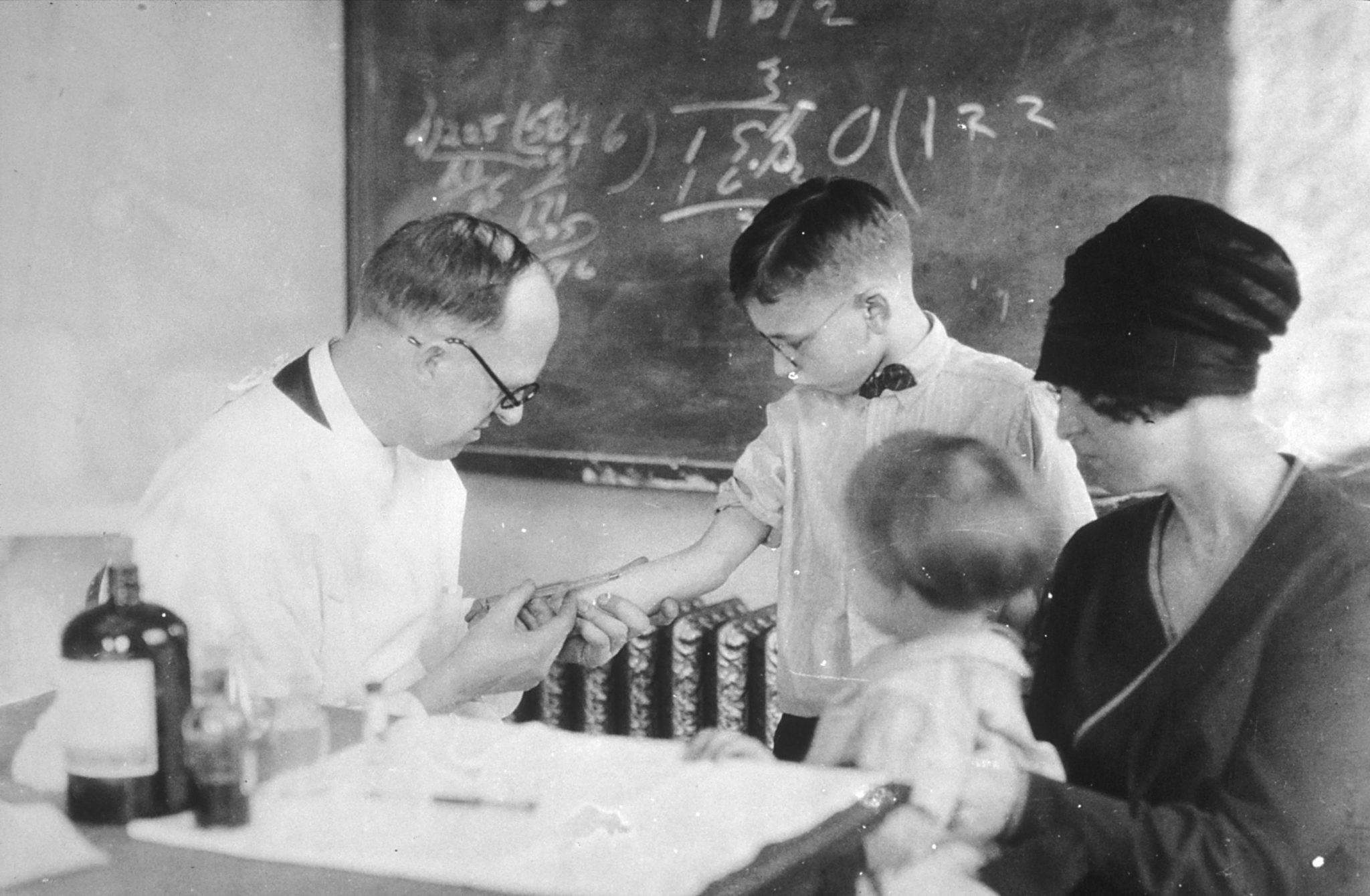
[Image: U.S. Hygiene Laboratory photo of Schick test, a measure of immunity from diphtheria, 1915]
It may be the weather, the economy, or the mounting pressure on hospitals and physicians to “compete” with each other like never before, but lately I have noticed a sharp increase in matters presented to me involving “professional review activities” by hospitals against physicians on their medical staffs. These disputes come in all shapes and sizes, but always require reference to the hospital\’s medical staff bylaws and applicable law.
In particular, the federal Health Care Quality Improvement Act of 1986 (“HCQIA”) provides for “safe harbor” procedures to be followed in the course of any professional review activity, compliance with which is a precondition to the legal immunities offered by the Act. The HCQIA\’s requirements have become the industry standard, and often shape (or at least must be read together with) the provisions of a hospital\’s medical staff bylaws concerning the due process rights of affected practitioners.
In 2004, a jury in the Northern District of Texas awarded a physician $366 million in damages against a hospital and members of its medical staff for action taken by them to suspend the plaintiff physician\’s medical staff privileges. The award in that case, Poliner v. Texas Health Systems, et al, sent shivers through hospitals throughout the country because the trial court permitted the damages award to stand (albeit substantially reduced in amount on remittitur), notwithstanding the defendants\’ claim of immunity under the HCQIA. This week, the Fifth Circuit Court of Appeals issued a decision in the defendants\’ appeal on this issue, and reversed the judgment of the District Court.
The Court\’s opinion focused on whether the defendants in Poliner had adhered to the four requirements for immunity under the HCQIA:
1 – Were their actions taken in the reasonable belief that they furthered quality health care?
2- Was there a reasonable effort to obtain the facts?
3- Were adequate notice and hearing procedures afforded to the affected physician?
4- Did they reasonably believe that their adverse action was warranted by the facts known?
There was no dispute that these were the requirements for immunity under the HCQIA. The question faced by the Fifth Circuit was whether the District Court had interpreted these requirements correctly in applying them to the defendants in Poliner. In several important respects, the Fifth Circuit found that the District Court had erred.
Of most importance to hospitals and counsel for physicians on both sides of these situations, the Fifth Circuit held:
– The HCQIA\’s reasonableness requirements were intended to create an objective standard of performance rather than a subjective good faith standard.
– The Court\’s review of the reasonableness of the defendants\’ decisions must be based on the information known to them at the time, and not what might be later shown to be true by experts or otherwise.
– Immunity does not require the defendants to have been correct or “right” in their findings, only that their findings were objectively reasonable under the facts available at the time.
– Plaintiff\’s allegations of anti-competitive motives and evil intent are of no consequence to the immunity offered by the HCQIA if the defendants\’ actions are objectively reasonable.
– Immunity from money damages under the HCQIA does not require compliance with the hospital\’s medical staff bylaws, as long the four requirements of the HCQIA set forth above have been met.
This decision will greatly affect the resolution of conflicts involving professional review action, whether during the hospital-medical staff proceedings or in subsequent litigation. The trial court\’s decision created a perception of risk in many professional review scenarios that expanded the range of potential outcomes “on the table” during any effort to resolve these matters. Under the Fifth Circuit\’s decision, that range has been shrunk.
Aside from its value as direct precedent, the decision is very clear, well reasoned and practical in its approach, and I wager it will be widely followed. Affected physicians will now get far less impact from suggestions that “the review panel was out to get me,” “my expert knows more about this than you do,” or “the hospital didn\’t follow its bylaws.”
Poliner appears to have put the balance of negotiating power back to where it was intended by the HCQIA. It clearly elevates considerations of patient safety over the right of an affected physician to seek money damages. It leaves unchanged the affected physician\’s right to seek remedies other than money damages (e.g., to enforce rights under the medical staff bylaws), and holds hospitals and medical staffs to a reasonable standard of conduct that they can realistically implement. It warrants their collective sigh of relief.
(Hat tip to the Horty Springer Health Law Express (join here) for being the first to bring this decision to my attention.)
